In Arizona alone, nearly 600,000 adults are living with diabetes and one in every three adults is completely unaware they have pre-diabetes, a condition in which your body does not properly respond to insulin resulting in higher than normal blood sugar. Over time, having too much glucose in your blood can cause health problems, such as heart disease, nerve damage, eye problems and kidney disease.
Alarmingly, the rate of patients with Type 2 diabetes in the state has doubled in the past decade. Mission of Mercy is at the front lines of this battle. Approximately 80% of the patients who visit a Mission of Mercy (MOM) clinic site have one or more chronic conditions with the top three conditions being hypertension, diabetes and high cholesterol. MOM patients have a prevalence rate of diabetes of 44% – more than four times higher than the statewide average of 10.3%.
MOM’s volunteer physicians and nurses treat patients like Martha*, a 62-year-old grandmother of eight who is the primary caregiver for her 85-year-old mother and also helps with after-school care for several of her grandchildren. When she first came to a MOM clinic, she sought treatment for the seasonal flu virus. She was unaware that she was living with Type 2 diabetes.
Martha’s story is not unlike many MOM patients. Caring for Arizona’s uninsured and under-insured populations is exactly what the nonprofit has been doing for the past 22 years. Most patients earn too much to qualify for AHCCCS (Medicaid) and/or too little to afford private insurance.
“Our patients have very limited budgets and as a result, they put their health at the very bottom of their priority list,” said MOM Medical Director Brad Smith, NMD. “Unfortunately, many patients can’t even afford the cheapest medications, let alone money for food, the electric bill or transportation.”
Piloting a program to tackle root causes
MOM recently secured significant grants from Dignity Health St. Joseph’s Hospital and Medical Center as well as Blue Cross Blue Shield of Arizona’s (BCBS) Mobilize AZ program to address this growing problem and improve the health of uninsured patients with diabetes.
Because uninsured diabetes patients have 60% fewer physician office visits and are prescribed 52% fewer medications than people with insurance coverage, the result is they make 168% more emergency department visits than people who have insurance. This places a heavy strain on our healthcare system, driving up costs for everyone.
The pilot diabetes management program that launched at MOM’s North Phoenix and Maryvale clinic locations with initial support from BCBS and Dignity Health gives patients the tools they need to succeed, thereby keeping them out of emergency rooms and improving their overall quality of life.
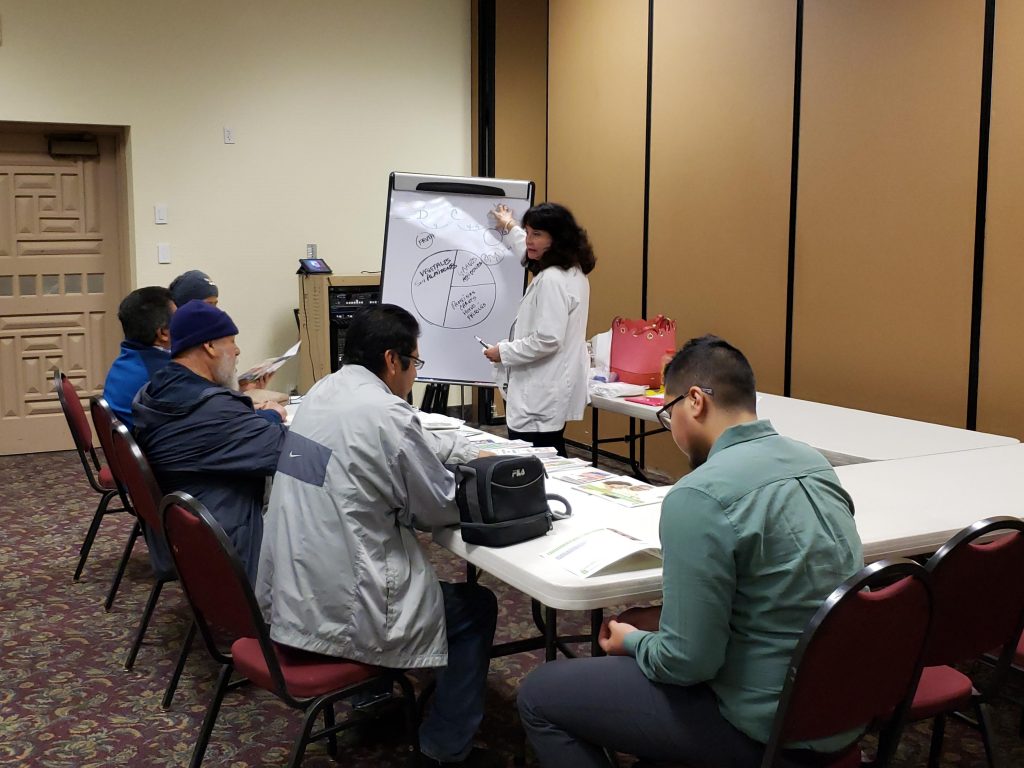
“We are building a network of support for our patients with many needs, which gives them the knowledge and confidence to make positive lifestyle changes that will improve their health outcomes. We have the opportunity to share in both their successes and challenges,” said Cecilia R. Chapman, RDN, CDE (bilingual Registered Dietitian Nutritionist and Certified Diabetes Educator). “We celebrate every success, no matter how small. And if numbers aren’t heading in the right direction, I am able to counsel patients individually to identify needed changes. These can be as simple as cutting soda out of their diet or taking a walk once a week. And we build on their small victories every visit, so they don’t feel overwhelmed.”
The grants provide funding to help patients with diabetes by providing six clinic visits per year to track weight, blood pressure, body mass index (BMI) and HbA1c levels (a critical measurement for diabetic patients), along with providing personal counseling for individuals and small group diabetes sessions, lab work and prescription medications. The grants also provide funds for a point-of-care HbA1c analyzer, which helps MOM clinicians more effectively assess patients and manage their care in a timely fashion.
Increasing patient compliance
MOM’s diabetes management program also includes an innovative partnership with Gregory’s Fresh Market to provide diabetic patients with access to 10 pounds of fresh produce via an on-site farmer’s market at the clinic six times during the grant period. Nutritional information is provided as well as cooking demos that show how patients can incorporate fresh produce into their daily diet.
“Compliance is the key to improving one’s health when faced with diabetes, and it’s the hardest thing to do,” Dr. Smith said. “While prescription medications are one part of the equation, diet and exercise play a huge role in a diabetic patient’s treatment plan. With a Certified Diabetes Educator on our team, we are seeing patients be more accountable for their role in leading a healthier lifestyle.”
Ultimately, the goal of these programs is to improve patient outcomes so it can be replicated at MOM’s five other mobile clinic locations. But in order to do that, additional funding is needed to support a larger capacity.
“We’re always seeking funders who have a passion for community healthcare and are committed to making tangible improvements in the lives of those less fortunate,” said MOM Executive Director Paula Carvalho. “Blue Cross Blue Shield and Dignity Health have helped provide a launching pad for what we hope will become a larger platform of support for our patients dealing with diabetes.”
*Patient name has been changed to protect privacy.
Sources: Arizona Department of Health Services, Centers for Disease Control and Prevention, American Diabetes Association